I am a great believer in luck, and I find the harder I work, the more I have of it.
-- Thomas Jefferson
I started to write this post about two months ago. I had collated a ton of information on questions to ask when you're headed into an induction. Then my computer crashed, and I lost all of it, and I haven't had the motivation to write it again.
Until a few weeks ago, when I got a text from my good friend "N." After months of preparing for a med-free childbirth, she was facing a medically-necessary induction, and was wondering if I had any tips? Gee, it would've been nice to be able to point her to that blog post...
As it turns out, N didn't need it: She made it through her induction epidural-free and birthed her baby girl vaginally. But with induction rates soaring, there are still a lot of women out there who do need this information.
I see a lot of commonalities between N's labor/birth and mine with Littles. We both got lucky, for sure. One of the things that really struck me about Littles' birth was how little control I had over the process. It was up to my body to do its thing, or not do its thing. Thankfully -- luckily -- it did.
But I don't think my successful induction, or N's, was due to pure luck. We both worked hard to be that lucky. There is nothing a woman can do to guarantee a successful induction, but there are certainly some things she can do to up her chances of it.
Namely, ensuring that she has answers to a couple of key questions.
Do I have the support that I'll need?
A successful induction starts long before the induction. In retrospect, three keys to my induction were in place many weeks before I found out I would be induced:
- I educated myself -- and perhaps more importantly, my husband -- on birth and birth options via childbirth preparation classes.
- I talked over my birth plan with my OB, and ensured that she was on the same page.
- I hired a doula.
Many people say that these things aren't important, and for some labors, that's true: I probably could have gotten through my two-hour labor with Q without any of that in place. But inductions can be challenging -- Littles' certainly was! And so having that support in place can make a huge difference in the outcome.
In fact, if you have that kind of support lined up already, you could probably skip the rest of this post. You won't have to ask a whole lot of questions before/during your induction, because the people around you will automatically shepherd you in the right direction. Indeed, my friend N had great support as well: She birthed at the awesome hospital where I originally planned to have Noob, she took Bradley classes with her fabulous husband, she hired M (who attended my last two births) as her doula. So when she texted me to ask for advice heading into her induction, I gave her a few quick pointers, but trusted that I didn't need to say a whole lot. She already knew most of what I'm about to write, and I was confident that her husband or OB or doula or L&D nurse would help with the rest.
What are the risks of an induction?
Even the most necessary of inductions carries some risk. This goes back to my key #1 above: If you've taken a good childbirth prep class, you're probably well aware of these risks. If you haven't, ask your OB. If your OB tells you that there are no risks... do some research on your own. M (my doula) has a great blog post that will get you started.
Why am I being induced?
Hopefully, you don't even need to ask this question, because you and your provider are communicating well and you fully understand the reasons behind his/her recommending induction. But if you're unsure, well, you'll want to clarify whether you're being induced for urgent medical reasons or just because your provider is going on vacation.
Can we wait to induce for another day? Two days? Three days? Longer?
Every day your baby stays inside is another day for him/her to develop, and another day for your body to prepare for labor. (Or even go into labor on its own!) Even so, sometimes, babies reach the point where they are safer out than in and really need to be induced ASAP. But it's worth clarifying whether this is the case with your baby or if you could wait another couple of days (or weeks?) to induce.
What is my Bishop score?
Your Bishop score takes into account the dilation, effacement, consistency, and position of your cervix, along with your fetal station.
The higher your Bishop score, the higher your chance of a successful induction. Bishop scores of 9 or higher are associated with the greatest chance of induction succeeding.
Your Bishop score should be weighed against the answers to the previous two questions. If you have a low Bishop score but you're being induced for solid and urgent medical reasons, you should start with cervical ripening and hope for the best. But if you have a low Bishop score and you're considering an elective induction... well, you might want to give some serious thought as to whether that is the right course of action.
If I need cervical ripening, will you use Cytotec?
If you need to be induced despite a low Bishop score (5 or lower), your provider should recommend cervical ripening first, before starting Pitocin. There are a variety of methods for achieving cervical ripening, including a foley catheter, Cervidil (prostaglandin E2 gel), and Cytotec (misoprostol).
Cytotec is a favorite villain of the natural birth community, primarily for these three reasons:
- Cytotec is not FDA-approved for labor induction. Induction is an "off-label" usage.
- There have been reports of uterine rupture after using Cytotec to induce labor.
- As a result of #1 and #2, Searle (the former manufacturer of Cytotec) sent a letter to doctors warning them not to use Cytotec to induce labor.
While all of these criticisms are true, they do not give the full story:
- Regarding Cytotec's "off-label" usage, doctors prescribe drugs off-label all the time. It is not necessarily dangerous or sinister. Case in point: I've mentioned previously that I took progesterone supplements (specifically Prometrium) during the first trimester with both Noob and Q. Prometrium is FDA-approved for hormone replacement therapy in menopausal women; pregnancy is listed as a contraindication. Yet it's commonly prescribed "off-label" for pregnant women with low progesterone, and I credit it with saving both Noob's and Q's lives.
- Regarding the reports of uterine rupture, they occurred primarily in women attempting VBAC (vaginal birth after cesarean). Certainly, Cytotec should never be used in women with a history of uterine surgery. But for women without such a history, the risk of uterine rupture with Cytotec is similar to what it is during a spontaneous labor.
- Regarding Searle's letter, it was primarily a "cover your ass" move, to absolve the company of any responsibility for adverse outcomes resulting from off-label use of the drug. Again, it does not mean that this off-label use is dangerous or sinister.
- Cytotec has been shown to be more effective than other methods of cervical ripening. Women induced with Cytotec are less likely to need other interventions, such as Pitocin or a c-section. See, for example, this study and this study.
All that said, when I was facing induction, I specifically talked to Dr. S and Dr. K about avoiding Cytotec. There are two things that I don't like about Cytotec:
- It is a pill that you take either orally or vaginally. If it does cause uterine hyperstimulation, which is a known risk, you cannot remove it (like you can with Cervidil) or turn it off (like you can with Pitocin). You just have to wait for the dose to dissipate and hope your uterus doesn't rupture in the meantime.
- A Cytotec pill contains 100 micrograms of misoprostol. The recommended dose is 25 micrograms. This means that the pill must be cut into quarters before administration to the patient. Since the medication may not be dispersed evenly across the pill, a quarter of a pill could contain 25 micrograms of misoprostol... or 0 micrograms... or 100 micrograms. You just don't know.
Bottom line, there are benefits and risks to Cytotec. Informed consent is key. Ask your provider if s/he plans to use Cytotec, and if s/he does, have a conversation about those benefits and risks so you can decide if Cytotec is right for you.
How do you see my induction unfolding, as far as which induction mechanisms at what time?
Most providers will have women who need cervical ripening (Cervidil, Cytotec, foley catheter, etc.) come in the night before the actual induction to get started with that. For example, my Monday induction started with Cervidil on Sunday night.
If your cervix is already ripe, your provider will likely have you come in on the morning of your induction to get started with Pitocin, amniotomy (breaking your bag of waters), etc.
You should talk over the "schedule" with your provider, as well as discuss which induction mechanisms s/he plans to use and why. For example, if your provider plans to induce you via amniotomy, you might want to talk about whether that will put you "on the clock" (many providers want women to deliver within a certain time frame after their bag of waters is broken, usually about 24 hours), when and why s/he might decide that you need Pitocin to move things along, the risk of infection, etc.
Will I be able to eat/drink freely during my induction?
I already wrote a whole post on eating and drinking during labor, but it is even more relevant to an induced labor because inductions can take a long time. And unlike a spontaneous labor, where you can labor at home (and therefore eat and drink freely) for much of your labor, an induced labor typically takes place entirely in the hospital. I've had friends who have had 2- and 3-day inductions where they were allowed nothing but ice chips. That seems borderline cruel to me!
As I pointed out in the other post, there is really no good reason for hospitals to restrict food during any labor, induced labors included. With Littles, my hospital brought me breakfast on the morning of my induction, after the Cervidil was removed but before starting Pitocin. If your hospital isn't as progressive, consider sneaking some snacks to keep your energy levels up.
What sort of fetal monitoring will I need?
Most hospitals require continuous electronic fetal monitoring (EFM) for women being induced. This is for good reason: One of the big risks of induction is that it can be too effective, causing uterine hyperstimulation, potentially leading to fetal distress, uterine rupture, etc. EFM can help detect this situation before it becomes an emergency.
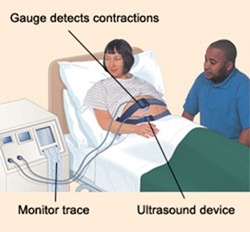
Normally, EFM requires two large belts to be strapped to your abdomen (one to monitor the baby's heart rate, another to monitor your contractions) and hooked up to a machine:
Obviously, this greatly limits your freedom of movement... but you can still move around while on EFM. I certainly wasn't walking the hospital halls during my induction, but I was able to sit on the edge of the bed, sit on a birthing ball, sit in a chair, stand up, squat, etc. Good thing, because lying in bed was absolutely excruciating for me. If I hadn't been allowed to move into other positions, I don't think I would have lasted more than an hour or two without an epidural. And if I had gotten an epidural, then I wouldn't have been able to move into other positions. My body was already at a disadvantage, trying to birth a nine and a half pound baby who was not necessarily ready to come out, without the benefit of all the spontaneous-labor hormones that would have prepared my body to help her come out. Being stuck in bed would have put my body at even more of a disadvantage.
Despite all this, many doctors require women to stay in bed while on EFM. As far as I can tell, there is no good reason for this. The only problem that moving around caused me was that the belts would slip and lose Littles' heartbeat. This meant that a nurse had to come in every few minutes to readjust the belt and pick up her heartbeat again -- inconvenient for her, I'm sure, but, well, it was her job. My job was to get my baby out. We both did our jobs, and I absolutely believe that contributed to the positive end result.
So, if you'll be on EFM during your induction, don't let them stick you in bed! Talk to your OB about moving around within the limits of the EFM machine. Also, ask if your hospital has wireless telemetry units. These allow for fetal monitoring while giving you complete freedom of movement. You can even go in the tub with one on! But not all hospitals have them, and those that do sometimes don't have enough for every laboring woman -- so it's good to know ahead of time whether it's an option for you, and to express your interest in using one if possible.
I wanted to birth without pain medication. Now that I'm being induced, is this still possible?
This isn't a question for your provider, but for yourself. And the answer is an unequivocal YES. You have to believe that you can do it... because you can.
Back when I was pregnant with Littles, I heard very few stories of pain-med-free inductions. Even my doula admitted (after the fact) that I was her first client to make it through an induction without an epidural. Now I hear those types of stories all the time. Women are doing it. You can do it.
I've done everything "right." Does that mean I'm going to have a wonderful, easy vaginal birth?
Unfortunately, no :( It might not be any of those things. That's labor for ya. Jefferson said that the harder he worked, the luckier he was -- not that he was lucky all the time.
But for me, this goes back to my birth mindset. I had a sense of peace when I showed up at the hospital for my induction. Induction wasn't what I had hoped for, but I knew that it was the safest, most informed decision under the circumstances. I knew that I had asked all the right questions. I knew I had a great support team surrounding me. And so that sense of peace came from knowing that I was headed for the best possible outcome. Again, not necessarily the outcome I had hoped for (that is pure luck)... but the best possible outcome regardless.
It's my hope that every woman headed into an induction -- or into spontaneous labor, or into a scheduled c-section, for that matter -- has that sense of peace, and achieves her best possible outcome as well.